Study links congenital heart disease to oil, gas development by Tauren Dyson, July 18, 2019, UPI
AURORA, Colo.(July 18, 2019) – Mothers living near more intense oil and gas development activity have a 40-70% higher chance of having children with congenital heart defects (CHDs) compared to those living in areas of less intense activity, according to a new study from researchers at the Colorado School of Public Health.
“We observed more children were being born with a congenital heart defect in areas with the highest intensity of oil and gas well activity,” said the study’s senior author Lisa McKenzie, PhD, MPH, of the Colorado School of Public Health at the University of Colorado Anschutz Medical Campus. At least 17 million people in the U.S. and 6% of Colorado’s population live within one mile of an active oil and gas well site.
The study was published today in the peer-reviewed journal Environment International.
The researchers studied 3,324 infants born in Colorado from 2005-2011. They looked at infants with several specific types of CHDs.
Researchers estimated the monthly intensity oil and gas well activity at mother’s residence from three months prior to conception through the second month of pregnancy. This intensity measure accounted for the phase of development (drilling, well completion, or production), size of well sites, and production volumes.
They found mothers living in areas with the most intense levels of oil and gas well activity were about 40-70% more likely to have children with CHDs. This is the most common birth defect in the country and a leading cause of death among infants with birth defects. Infants with a CHD are less likely to thrive, more likely to have developmental problems and more vulnerable to brain injury.
Animal models show that CHDs can happen with a single environmental exposure during early pregnancy.
Some of the most common hazardous air pollutants emitted from well sites are suspected teratogens – agents that can cause birth defects – known to cross the placenta.
The study builds on a previous one that looked at 124,842 births in rural Colorado between 1996-2009 and found that CHDs increased with increasing density of oil and gas wells around the maternal residence. Another study in Oklahoma that looked at 476,000 births found positive but imprecise associations between proximity to oil and gas wells and several types of CHDs.
Those studies had several limitations including not being able to distinguish between well development and production phases at sites, and they did not confirm specific CHDs by reviewing medical records.
The limitations were addressed in this latest study. Researchers were able to confirm where the mothers lived in the first months of their pregnancy, estimate the intensity of well activity and account for the presence of other air pollution sources. The CHDs were also confirmed by a medical record review and did not include those with a known genetic origin.
“We observed positive associations between odds of a birth with a CHD and maternal exposure to oil and gas activities…in the second gestational month,” the study researchers said.
The study data showed higher levels of CHDs in rural areas with high intensities of oil and gas activity as opposed to those in more urban areas. McKenzie said it is likely that other sources of air pollution in urban areas obscured those associations.
Exactly how chemicals lead to CHDs is not entirely understood. Some evidence suggests that they may affect the formation of the heart in the second month of pregnancy. That could lead to birth defects.
McKenzie said the findings suggested but did not prove a causal relationship between oil and gas exploration and congenital heart defects and that more research needs to be done.
“This study provides further evidence of a positive association between maternal proximity to oil and gas well site activities and several types of CHDs,” she said.
“Taken together, our results and expanding development of oil and gas well sites underscore the importance of continuing to conduct comprehensive and rigorous research on health consequences of early life exposure to oil and gas activities.”
The study co-authors include William Allshouse, PhD, BSPH and Stephen Daniels, MD, PhD, both of the University of Colorado Anschutz Medical Campus. The study was funded by a grant from the American Heart Association.
Refer also to:
Frac’ing could threaten air quality, workers’ and public health, University of Maryland report says
Arvin California: Expert Says Independent Air Sample of Evacuated Home Shows Relatively High Levels of Chemicals Linked to Hydraulic Fracturing
Study: Toxic Chemicals, Carcinogens at Levels Far Exceeding Federal Limits Near Frac Sites, Will almost certainly lead to cancer increase in surrounding areas
Want a job that kills babies? New Study in Pennsylvania: Fracking strongly related to increased mortality in young babies – Polluted well water is likely cause
Another New Study Showing Frac Harm: ‘Fracking’ Linked to Low Birth Weight Babies, Pregnant women who live near multiple natural gas wells tend to have smaller infants
Pennsylvania Study Links Fracking to Health Hazards in Fetuses, Infants, Young Children: 35.1% more cancer in children ages zero to four in heavily frac’d counties. Compare to AER’s belittling, dismissive health study in the Lochend
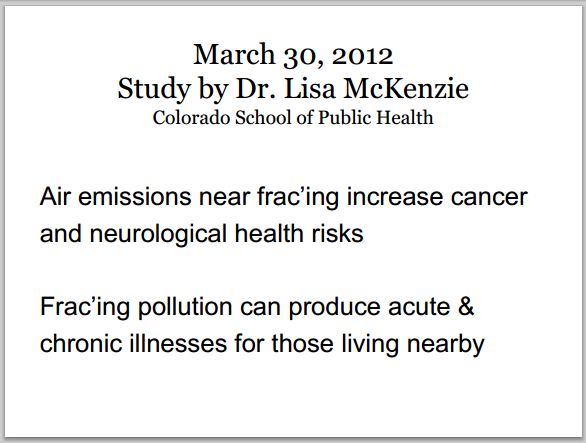
New peer-reviewed, published study by Lisa McKenzie et al, U Colorado School of Public Health: Childhood cancer linked to nearby oil and gas activity; People ages 5-24 diagnosed with acute lymphocytic leukemia more likely to live in areas with a high concentration of oil and gas activity
NE BC Fracking May Be Exposing Pregnant Women to Carcinogen, Study Says; Researchers found markers suggested benzene levels 3.5 times normal levels
New Study on Pregnant Women Living Near Frac’d Natural Gas Sites in Peace River Valley, NE BC Raises Concerns: Benzene biomarker (muconic acid) in urine 3.5 times higher than in women in general Canadian population
Colorado Investigates a Spike in Fetal Abnormalities Near Natural Gas Drilling Site, A prevalence of anomalies such as low birth weight and congenital heart defects are found within a 10 mile radius of a concentration of gas wells
Des malformations congénitales liées à l’extraction du gaz naturel; New study links fracking to birth defects in heavily drilled Colorado, Risks of some birth defects increased as much as 30 percent in mothers who lived near oil and gas wells
Queensland Australia: Another new study shows unconventional gas industry pollution: Air Pollution and human health hazards: a compilation of air toxins acknowledged by gas industry in Queensland’s Darling Downs. As expected and as usual, industry name calls the scientist, Geralyn McCarron, “activist” to try to discredit her and her alarming paper
Alberta Energy Minister Margaret McCuaig-Boyd deflecting the known frac risks and harms? Says “fracking affects regions differently,” wants to “wait until we get the science going” before making any decisions even though the science on fracing is already in.
Compendium 6 Released: Review by doctors & scientists of more than 1,700 references conclude frac industry poses threat to air, water, climate and human health